An irregular heartbeat, known as arrhythmia, occurs when the heart’s rhythm is abnormal. It can manifest as an abnormally slow heartbeat or an unusually rapid one (often causing heart palpitations).
The Department of Veterans Affairs (VA) assigns disability ratings for arrhythmia at four levels: 10%, 30%, 60%, or 100%. These ratings are determined based on how severe the condition is, how long it lasts, and how often symptoms occur.
How the VA Rates Different Types of Heart Arrhythmias
Supraventricular Arrhythmias (Diagnostic Code 7010)
This includes conditions like atrial fibrillation, atrial flutter, and paroxysmal atrial tachycardia.
- 30%: Paroxysmal atrial fibrillation or other supraventricular tachycardia, with more than four treatment interventions per year and documented by ECG or Holter monitor
- 10%: one to four treatment interventions per year of paroxysmal atrial fibrillation or other supraventricular tachycardia documented by ECG or Holter monitor; or confirmed by ECG with either continuous use of oral medications to control or use of vagal maneuvers to control
A treatment intervention occurs whenever a symptomatic patient requires intravenous pharmacologic adjustment, cardioversion, and/or ablation for symptom relief.
Premature Atrial Contractions (PACs)
The VA disability rating for Premature Atrial Contractions (PAC) is typically evaluated under Diagnostic Code 7010, the same as for Supraventricular arrhythmias. See the ratings.
Some people who have PACs turn out to have related heart conditions, such as Cardiomyopathy, which is a disease of the heart muscle that makes it harder for the heart to pump blood to the rest of the body.
Ventricular Arrhythmias (Sustained) (Diagnostic Code 7011)
This includes conditions like ventricular tachycardia. Ventricular arrhythmias are evaluated according to VA’s general rating formula for heart diseases.
General Rating
-
100% for indefinite period from date of hospital admission for initial evaluation and medical therapy for a sustained ventricular arrhythmia
or for indefinite period from date of hospital admission for ventricular aneurysmectomy
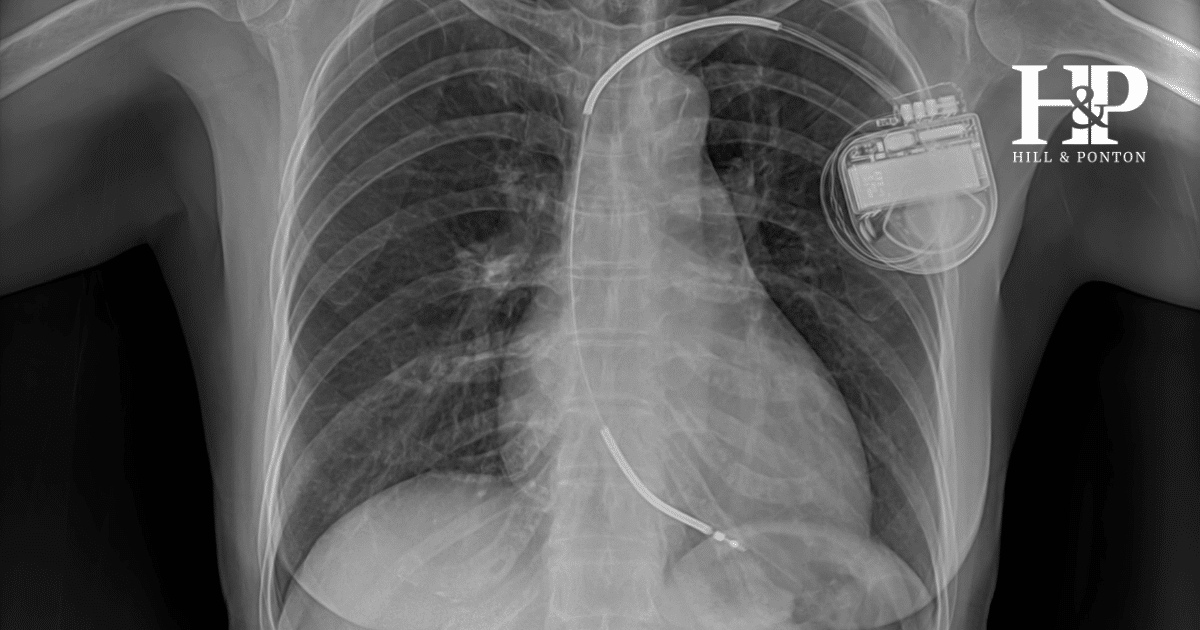
or with an automatic implantable Cardioverter-Defibrillator (AICD) in place - 100% with a workload of 3.0 METs or less resulting in heart failure symptoms
- 60% for 3.1-5.0 METs resulting in heart failure symptoms
- 30% for 5.1-7.0 METs resulting in heart failure symptoms; or evidence of cardiac hypertrophy or dilatation confirmed by echocardiogram or equivalent (e.g., multigated acquisition scan or magnetic resonance imaging)
- 10% for 7.1-10.0 METs resulting in heart failure symptoms; or continuous medication required for control
Premature Ventricular Contractions (PVCs)
The VA disability rating for Premature Ventricular Contraction is typically evaluated under Diagnostic Code 7011 for Ventricular arrhythmias (sustained). Ratings range from 10% to 100% based on the frequency of episodes, need for medication, and impact on daily activities. See the full ratings above.
Atrioventricular Block (Diagnostic Code 7015)
Benign Atrioventricular Block (First-Degree and Second-Degree, Type I) is evaluated according to the general rating.
Non-Benign Atrioventricular Block (Second-Degree, Type II and Third-Degree) is evaluated according to DC 7018 (implantable cardiac pacemakers) – see the ratings here.
Sinus Bradycardia/Tachycardia
These conditions are often rated analogously to other arrhythmias or based on their underlying cause.
See VA ratings for Sinus Bradycardia
See VA ratings for Sinus Tachycardia
VA will typically rate a heart condition based on its most predominant symptom or the diagnostic code that results in the highest rating. Additionally, some heart conditions may be rated under the general rating formula for diseases of the heart (Diagnostic Code 7000) if it better represents the veteran’s overall cardiac function.
Master the VA Disability Claims Process
When Does Arrhythmia Qualify for VA Disability?
Heart arrhythmia qualifies for VA disability when it is service-connected, meaning it was caused or aggravated by military service. Causes may include:
- Physical stress during service
- Exposure to toxins or chemicals
- Traumatic injuries affecting the heart
- Certain medications used during service
Can PTSD cause heart arrhythmia?
Yes, studies have shown a link between PTSD and increased risk of heart arrhythmias. The chronic stress associated with PTSD can lead to changes in heart rate and rhythm, palpitations, etc. Learn more about heart palpitations and PTSD.
Is Heart Arrhythmia a Presumptive VA Condition?
Heart arrhythmia is not a presumptive condition. It can however be connected to other conditions considered presumptive by the VA.
Chronic Diseases
Some heart conditions that can lead to heart palpitations and arrhythmias are considered chronic diseases under VA regulations. If these conditions manifest to a compensable degree within one year of discharge from active service, they may be presumptively service-connected. They include:
- Endocarditis (which covers all forms of valvular heart disease)
- Myocarditis
- Arteriosclerosis
- Cardiovascular-renal disease, including hypertension
While arrhythmia itself is not specifically listed, if it’s a symptom or result of one of these conditions, it could be service-connected secondary to one of these presumptive conditions if it includes symptoms not already compensated by the service-connected condition.
Radiation Exposure
While not specific to arrhythmias, some heart conditions can be presumptively service-connected for veterans exposed to ionizing radiation during service. If an arrhythmia is secondary to one of these conditions and includes symptoms not already compensated by the primary heart condition, it could be service-connected.
Former Prisoners of War (POWs)
For former POWs interned for any length of time, atherosclerotic heart disease and hypertensive vascular disease (and their complications, which could include arrhythmias) are presumptively service-connected if manifested to a degree of disability of 10 percent or more at any time after discharge.
Even though a veteran’s heart arrhythmia is not a presumptive condition, a veteran can still claim it as a VA disability through direct service connection or secondary service connection – if they can provide evidence linking their condition to their military service or to another service-connected condition.
How to Service Connect Heart Arrhythmia
To service connect this condition, you need to provide:
- Current diagnosis of heart arrhythmia
- Evidence of an in-service event, injury, or illness
- Medical nexus linking the current condition to service or a service-connected condition.
How to File Your VA Claim
- Gather all relevant medical records
- Complete VA Form 21-526EZ
- Submit claim online through eBenefits, by mail, or in person at a VA regional office
- Include a detailed personal statement about how arrhythmia and its symptoms (such as breathlessness and palpitations) affect your daily life
Increase the VA Rating
- Gather new medical evidence showing worsening condition
- Request a new C&P exam
- Submit evidence of increased frequency or severity of episodes
- Provide documentation of how arrhythmia impacts work and daily activities
Get Help With Your VA Disability Claim
Secondary Conditions
The Department of Veterans Affairs (VA) recognizes several health problems that might develop as a result of or in connection with heart arrhythmia.
- Heart failure: Persistent arrhythmias can weaken the heart over time, potentially leading to heart failure.
- Cognitive impairment: Some studies have linked arrhythmias to an increased risk of cognitive decline and dementia.
- Anxiety and depression: Living with a chronic heart condition like arrhythmia can contribute to mental health issues.
- Sleep apnea: There’s a bidirectional relationship between sleep apnea and arrhythmias, with each condition potentially exacerbating the other.
- Hypertension: Some arrhythmias can lead to or worsen high blood pressure.
- Cardiomyopathy: Certain types of arrhythmias can lead to weakening of the heart muscle over time.
- Thromboembolism: The risk of blood clots in other parts of the body may increase due to arrhythmias.
- Syncope (fainting): Some arrhythmias can cause sudden drops in blood pressure, leading to fainting episodes.
VA Disability Rating for CAD Secondary to Ventricular Cardiac Arrhythmia
Coronary Artery Disease (CAD) can develop as a result of long-term arrhythmia. You will need to provide medical evidence linking CAD to your service-connected arrhythmia in order to obtain benefits. Find out more about CAD.
VA Disability Rating for Heart Stent Secondary to Ventricular Cardiac Arrhythmia
If you required a heart stent due to complications from a service-connected arrhythmia, you may be eligible for additional compensation. Document the medical necessity of the stent, any symptoms which aren’t compensated by your already service-connected heart conditions, and the relationship between the stent and your arrhythmia.
VA Disability Rating for Sleep Apnea Secondary to Ventricular Cardiac Arrhythmia
Sleep apnea can trigger arrhythmias, and some arrhythmias can worsen sleep apnea. If you develop sleep apnea after your arrhythmia diagnosis, consider filing for secondary service connection with supporting medical evidence.
Get Help with Your Claim
Has the VA denied your claim? Or is your rating lower than it should be? Did your irregular heartbeat and palpitations worsen over time? Get in touch with our attorneys!
Maximize Your Benefits
Unhappy with your VA decision? We’re here to help. Contact us for a free review of your case.