Kidney disease is a serious medical condition that can affect your overall health. If you have kidney disease that resulted from your time in military service, you may be eligible for benefits through the Department of Veterans Affairs.
Here’s what veterans need to know about kidney impairment, how the VA rates kidney conditions, and how kidney disease may appear as a secondary condition to diabetes.
What Is Kidney Disease?
Kidney disease is a condition that impairs kidney function, affecting the body’s ability to filter the blood, control blood pressure, and regulate other body systems. Impaired kidneys are unable to filter out waste, which can cause the buildup of waste and fluid. This can then lead to serious health problems.
Types of Kidney Disease
Kidney disease is a broad term that can appear in several stages.
Acute Kidney Disease
Acute kidney disease, or acute kidney failure, occurs when the kidneys stop functioning suddenly. Symptoms of acute kidney failure typically appear within a few days and are often a result of another illness. Acute kidney failure is more likely to occur when an individual has another condition that requires hospitalization or intensive health care. This is a serious condition that requires immediate medical treatment.
Diabetic nephropathy
Diabetic nephropathy is the beginning of kidney disease. In a person with diabetes, it is a progressive kidney disease caused by damage to the capillaries in the kidneys’ glomeruli. Diabetic nephropathy is diagnosed when there is a presence of elevated urinary protein excretion (primarily albumin), and when there is no other type of renal disease presence.
We will go over the connection between diabetes and kidney disease in more depth below.
Chronic Kidney Disease
Chronic kidney disease (CKD), also known as chronic renal disease, is a progressive loss of kidney function over a period of months or years. Individuals with diabetes or high blood pressure are screened for kidney disease, and if undiagnosed for a long period, may already be at the chronic stage by the time it is diagnosed.
Chronic kidney disease is identified by a blood test for creatinine, which is a breakdown product of muscle metabolism. Higher levels of creatinine indicate a lower glomerular filtration rate (GFR) and, as a result, a decreased capability of the kidneys to excrete waster products from the blood.
There are 5 stages of kidney disease, each stage being determined by the glomerular filtration rate.
| Stage | GFR | Description |
|---|---|---|
| 1 | 90+ | Normal kidney function, but urine findings may point to possible kidney disease |
| 2 | 60-89 | Mildly reduced kidney function, with urine findings that point to kidney disease |
| 3 | 59-30 | Moderately reduced kidney function |
| 4 | 15-29 | Severely reduced kidney function |
| 5 | Less than 15 or on dialysis | Very severe or end-stage kidney failure |
All individuals with a GFR of less than 60 for 3 months are classified as having chronic kidney disease (Stage 3), regardless of whether or not kidney damage is present. The rationale for including these individuals is that reduction in kidney function to this level or lower represents loss of half or more of the adult level of normal kidney function, which may be associated with a number of complications such as the development of cardiovascular disease.
End-Stage Renal Failure
End-stage renal failure is the condition of individuals with chronic kidney disease, who require life-supporting treatments for kidney failure, such as renal replacement therapy (dialysis or kidney transplant). This is usually Stage 5 in the progression of kidney disease. At this point, the kidney can no longer filter the blood for wastes, and therefore the blood must be cleansed by an outside source (such as dialysis), so that the body does not accumulate dangerous toxins.

Getting a Diagnosis: Testing for Kidney Disease
If the presence of kidney problems is suspected, the physician will most likely start out with a simple urine test. A dipstick is used to measure how much protein (albumin) is present in the sample. If there is more than 30mg of albumin, kidney disease has most likely set in, and further testing is done to determine how far the disease has advanced.
Further testing—especially if the individual is diabetic—includes blood tests that measure the kidneys’ ability to filter the blood. The test results record blood urea nitrogen (BUN) and serum creatinine levels in the blood sample. High levels of either indicate that the kidneys are unable to properly filter the wastes in the blood. Creatinine is a byproduct of the muscle’s metabolism of energy. BUN is a waste product formed in the liver when protein is metabolized into its component parts (amino acids). BUN is released by the liver and carried to the kidneys, where it is filtered out of the bloodstream.
Blood tests may also include the glomerular filtration rate (GFR), which the physician can calculate based on the creatinine test, age, body size, ethnicity and gender. Specifically, it estimates how much blood passes through the glomeruli each minute. If the GFR is low, the kidneys are not working as well as they should. The various stages of kidney disease are based on the GFR of the individual.
What are considered to be normal kidney test results?
The healthy kidney does excrete small amounts of albumin, but the concentration is generally too low to be detected by the standard testing. Normal kidney testing results would reveal an albumin secretion rate of less than 30 mg, or an albumin-creatinine ratio of less than 30mg. Therefore, there is a base level of proteins that can be secreted by the kidneys which is considered normal (below 30mg per day). Anything over that amount, between 30 and 300mg, is considered abnormal, and called microalbuminuria. Proteinuria occurs when there is more than 300mg of excess proteins in the urine sample.
| Normal albuminuria | Less than 30mg |
| Microalbuminuria | 30 – 300mg |
| Proteinuria | More than 300mg |
How Does the VA Rate Kidney Disease?
If you’re a veteran with kidney disease, you may be eligible for disability benefits. The VA will consider several factors when rating this disease.
The VA rates kidney disease under the genitourinary system. There are two separate rating schedules: one for dysfunctions (§4.115a) and one for diagnoses (§4.115b). In most cases, the rating code for diagnoses will reference the dysfunctions rating code for proper evaluation of the severity of the condition.
For example – if you have chronic kidney disease, and now require regular dialysis, the VA is supposed to rate your condition under “Chronic renal disease requiring regular dialysis” (listed on the rating code for diagnoses, under # 7530). In addition, this particular rating code requires the VA rater to consider “renal dysfunctions” when evaluating your condition, under the dysfunctions rating schedule.
The VA rates chronic kidney disease primarily as a renal dysfunction, and has 5 rating percentages for this condition: 0 percent, 30 percent, 60 percent, 80 percent, and 100 percent. These percentages are based on:
- The amount of albuminuria present in a urine sample, with edema (swelling); AND/OR
- The amount of waste (BUN or creatinine)collected in a blood test; OR
- A rating of high blood pressure under the VA’s diagnostic code; OR
- Generalized poor health
How The VA Evaluates Disability Claims for Kidney Disease
The VA ratings for renal dysfunction are:
- 100%: “Requiring regular dialysis, or precluding more than sedentary activity from one of the following: Persistent edema and albuminuria; or, BUN more than 80 mg%; or, creatinine more than 8 mg%; or, markedly decreased function of kidney or other organ systems, especially cardiovascular.”
- 80%: “Persistent edema and albuminuria with BUN 40 to 80 mg%; or, creatinine 4 to 8 mg%; or, generalized poor health characterized by lethargy, weakness, anorexia, weight loss, or limitation of exertion.”
- 60%: “Constant albuminuria with some edema; or, definite decrease in kidney function; or, hypertension at least 40 percent disabling under diagnostic code 7101.”
- 30%: “Albumin constant or recurring with hyaline and granular casts or red blood cells; or, transient or slight edema or hypertension at least 10 percent disabling under diagnostic code 7101.”
- 0%: “Albumin and casts with a history of acute nephritis; or, hypertension non-compensable under diagnostic code 7101.”
As mentioned above, if you require regular dialysis for your end-stage kidney failure, you are entitled to a 100% rating, because one of the rating requirements for the 100% rating is regular dialysis. Alternatively, you are entitled to a 100% rating if:
- You are reduced to sedentary activity due to persistent swelling or albuminuria; OR
- Your blood tests show a BUN of more than 80mg or creatinine of more than 8mg; OR
- You have markedly decreased function of the kidney or other organ systems, especially cardiovascular issues
As another example: your doctor tells you that you now have Stage 3 kidney disease. You experience persistent swelling, some weakness, and you have no energy. Your recent blood work came back with the results of a BUN level of 45mg. These symptoms warrant an 80% rating, because you meet three of the rating criteria for an 80%. The full criteria for the 80% are as follows:
- You experience persistent edema and albuminuria with a BUN of 40 to 80mg, or creatinine of 4 to 8 mg; OR
- You experience generalized poor health characterized by lethargy, weakness, anorexia, weight loss, or limitation of exertion
Diabetes & Kidney Disease: What’s The Connection?
Many veterans will qualify for secondary service connection for their kidney disease. Specifically, this may occur when they have kidney disease secondary to diabetes.
Type II Diabetes is not only an increasingly prevalent condition among United States citizens, but also among the veterans who served during the Vietnam Era. In its Special 2000 Update, the Institute of Medicine (IOM) officially recognized Diabetes Mellitus II as a health effect of exposure to the chemical Agent Orange, and established it as a presumptively service-connected condition under the qualifying circumstances.
As any diabetic can tell you, diabetes is not an isolated disease. It affects the rest of the body in a number of damaging ways. One of these is kidney (renal) disease. According to the American Heart Association, renal disease is a common, often severe complication of diabetes. Likewise, according to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), diabetes is the leading cause of chronic kidney disease and kidney failure in the US, accounting for nearly 44% of new cases of kidney failure.
How Diabetes Affects The Kidneys
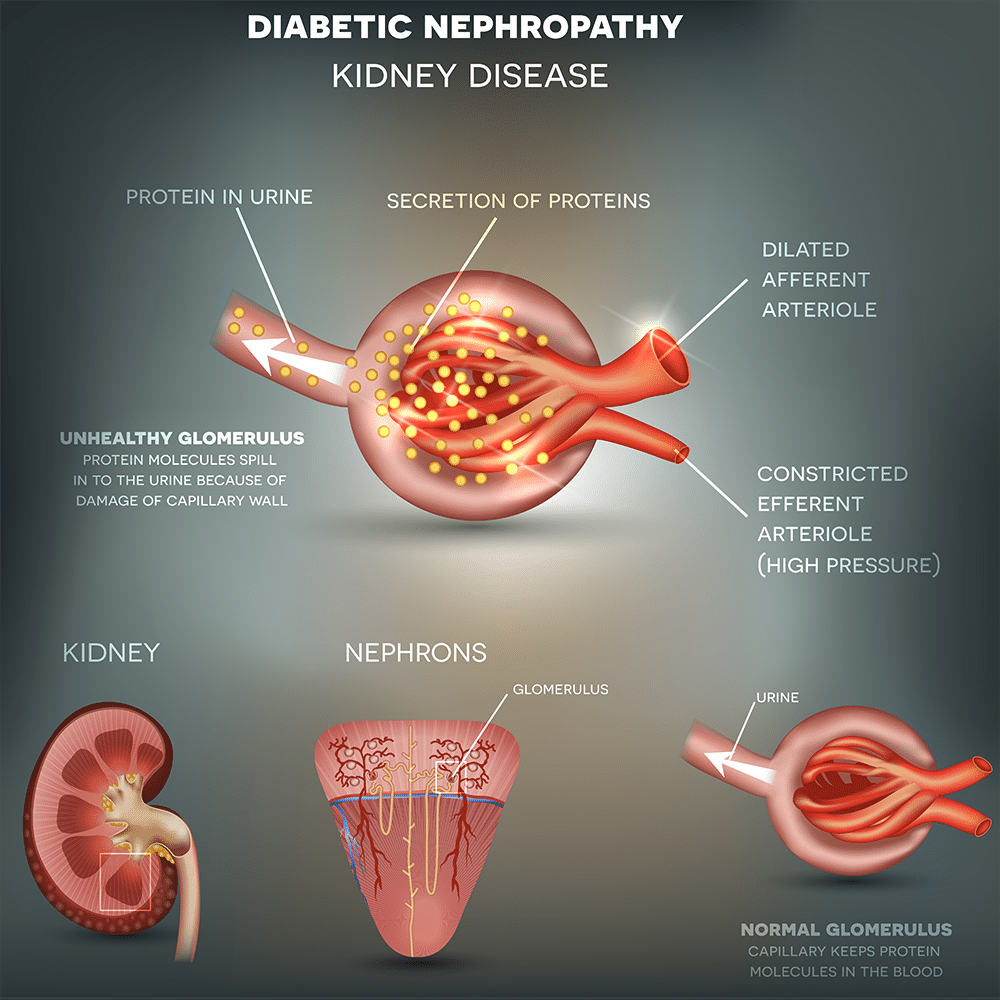
The kidneys are made up of hundreds of thousands of units called nephrons. These nephrons consist of a glomerulus and its attached tubule, which specializes in reabsorbing necessary fluids and secreting the rest as urine. Diabetes, particularly hyperglycemia, causes nephrons to slowly thicken and become scarred over time. The scarred nephrons begin to leak protein (albumin) into the urine. This is known as microalbuminuria. Albumin is an important component of human blood, as it transports hormones, fatty acids, and other compounds through the bloodstream. In a healthy kidney, the glomerulus normally secretes very small amounts of albumin. However, scarred nephrons allow too many albumin to slip through and pass into the secreted fluids, causing the body to lose these necessary proteins.
If caught early enough, slightly elevated levels of albumin in the urine will return to normal with proper control of blood sugar. However, after 7-15 years, 25% – 40% of insulin-dependent diabetics develop microalbuminuria, and the vast majority of these patients will progress to proteinuria over the following years. Development of persistent proteinuria often heralds a decline in renal function associated with even higher levels of protein excretion. In other words, proteinuria is a sign of chronic kidney disease (also called chronic renal failure).
Proteinuria occurs when there is a large excess of serum proteins in the urine. (This is not to be confused with microalbuminuria, which is a moderate increase of albumin in the urine.) Since serum proteins are readily reabsorbed from urine, the presence of excess proteins indicates either an insufficiency of absorption or impaired filtration of the kidneys. In either case, the loss of protein in the urine signals worsening kidney function and possibly cardiovascular disease.
Have Questions About VA Disability Benefits for Kidney Disease?
The VA’s schedule for rating disabilities can be complicated. If the VA denies your claim for benefits or awards fewer benefits than you expected, the legal team at Hill & Ponton can help. Our veterans disability attorneys can evaluate your entitlement for benefits, so you can earn the support you deserve. Contact us today to get started.