Peripheral neuropathy is an illness often linked to Agent Orange and herbicide exposure. It is associated with pain, burning, and numbness in the upper and lower extremities such as the hands and feet. It is presumptive for those veterans who served in Vietnam and were exposed to Agent Orange, however, only if it manifested within one year of exposure. You can read more about related Agent Orange diseases here. However many Gulf War veterans have also been exposed to similar agents, also known as organophosphates, in forms of pesticides, that have links to peripheral neuropathy. There are also several other toxins and illnesses that can lead to peripheral neuropathy as a primary or secondary condition. Veterans need to be aware that if they have peripheral neuropathy, there may be more than one reason and there could be a claim for service connection or secondary connection.
Toxin Exposures
Toxins associated with peripheral neuropathy are often thought of as being those Agent Orange and affiliate herbicides from the Vietnam era, including those used in Thailand, Guam, and even some US bases such as Anniston Army Depot in AL and Camp Pendleton in CA. Both these bases have been listed as EPA Superfund Cleanup Sites and one of the toxins listed is herbicides. Dozens of other bases, US and abroad, used pesticides that contained organophosphates linked to peripheral neuropathy (PN). However, again, these are linked to a specific type of neuropathy, one that manifests within a year or less. In order to be eligible for presumptive, or to have a good claim based on toxin exposure, there would need to be evidence of symptoms within a year of exposure. However, there are other ways that a veteran can get PN.
Diabetes Mellitus II
Most people are aware of the link between diabetes and PN. Diabetes causes blood to not reach the outer capillaries of the circulatory system, causing nerve damage in the feet, toes, hands, and fingers. As the damage increases with uncontrolled diabetes, the damage moves inward up the legs and arms and increases in pain levels. The neuropathy can lead to a person being unaware of wounds, causing infection and even leading to amputation.
Lupus and Autoimmune Diseases/Rheumatoid Arthritis
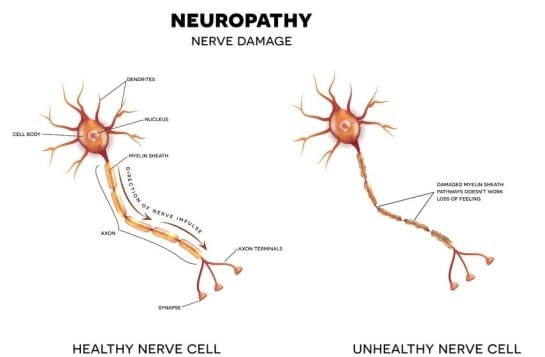
Many autoimmune diseases lead to PN. These diseases cause the body to attack its own tissue, often causing inflammation. That inflammation can often inflame the nerve fibers causing neuropathy. Some of these neuropathies can become severe and life-threatening such as Chronic inflammatory demyelinating polyneuropathy (CIDP) which damages the sensory and motor nerves. Autoimmune diseases are often found among Gulf War Veterans and some, such as MS, are presumptive for all veterans within a certain time frame from discharge.
Hyperthyroidism and Metabolic or Endocrine disorders
Diabetes is also a presumptive disease associated with herbicide exposure during Vietnam service. However, any veteran who was diagnosed with diabetes in service or whose diabetes manifested while on active duty is eligible for service connection. Veterans whose diabetes manifested within one year of discharge or who feel they were exposed to environmental toxins that may have been responsible for their diabetes are also welcome to file a claim, although they must be able to show a link between their service and their condition.
Diabetes is an endocrine disorder, but there are others that can also lead to PN. Hypothyroidism is another issue that is often seen in Gulf War veterans. Some metabolic liver conditions and hormonal imbalances can also cause PN. With thyroid conditions, underproduction of thyroid hormones slows the metabolism which leads to fluid retention and swollen tissue, putting pressure on peripheral nerves causing pain.
Small Vessel Disease
Diseases such as vasculitis cause blood vessel walls to harden, thicken, and develop scar tissue. When this happens, the vessels decrease in diameter and subsequently decrease the flow of blood to the peripheral extremities, leading to neuropathy in a similar fashion as diabetes. The lack of blood flow increased the nerve damage and it increases with time.
Kidney Disorders
Kidney disorders lead to increased levels of toxins in the blood that damage nerve tissues. Most people on dialysis have a form of neuropathy. The toxins damage the nerve fibers and the nerves are then unable to process signals correctly, leading to tingling, burning, pain, and numbness.
Cancers and Neuromas
Tumors, benign or not, and cancer cells, can increase pressure on nerve fibers depending on where they are growing, and can cause widespread pain. Treatment for cancer can also lead to extensive nerve damage as the chemotherapy medications and radiation kill nerve cells just as easily as cancer cells; 30-40% of people under cancer treatments have peripheral neuropathy and it is one of the leading reasons people stop cancer treatment earlier than recommended. Unfortunately, often stopping treatment does not stop or reverse the PN symptoms.
Infections
Several infectious diseases can cause PN such as those that attack nerve tissues. These include shingles, Epstein-Barr, West Nile, cytomegalovirus, and herpes simplex. Also, bacterial infections such as Lyme disease, diphtheria, leprosy are known for severe peripheral neuropathy issues. While diphtheria and leprosy are rare in the US, with our veterans traveling all over the world and often exposed to cultures that carry unknown diseases, there are risks. Lyme disease, shingles, and the other viruses are common in the US and can severely damage sensory nerves, causing pain, numbness, and may sometimes be permanent.
Medications
Not only do the medications used to treat cancer cause nerve damage, others do as well. Medications such as antiretroviral agents for HIV, some anticonvulsant agents, and some heart and blood pressure medications can cause PN. Check the side effects with your physician because often just adjusting the dosage can prevent the onset of PN.
Drug-Induced Peripheral Neuropathy
| Class | Drugs |
| Anticancer agents | Vinca alkaloids, taxane derivatives, platinum compounds, bortezomib, ixabepilone, lenalidomide, thalidomide |
| Antimicrobials | Chloroquine, colistin, dapsone, emtricitabine, ethambutol, isoniazid, itraconzole, lamivudine, linezolid, nitrofurantoin, tenofovir, voriconazaole |
| Cardiovascular agents | Amiodarone, digoxin, statins |
| Immunosuppressants | Interferons, leflunomide, penicillamine |
| Miscellaneous agents | Cimetidine, colchicine, levodopa, lithium, phenytoin |
Trauma, Injury, or Repetitive Stress
Sports-related injuries, auto accidents, surgical procedures….sometimes any type of trauma can cause the nerves to be damaged, crushed, impinged, or have pressure put on them in such a way that it impedes their ability to process signals correctly, leading to PN. Cumulative damage from repetitive use can often cause tendons to become inflamed, leading to pressure on the nerve fibers such as in the case of carpal tunnel syndrome.
PTSD and TBI
Recent studies have started to link PTSD to PN. Scientists are trying to find out the ways that PTSD may cause PN but there are several theories. Some include the body’s chemical reaction to stress and how those chemicals change the pituitary and adrenal glands, resetting the hormonal balance of our body. This, in turn, causes such issues as explained in the section above on hormonal and endocrine conditions. Another theory concerns neurochemicals such as serotonin, amino acids, and peptides, which may deregulate the way that nerve signals are translated. When parts of the brain are damaged by TBI or PTSD, such as the cortex, these neurochemicals become unbalanced and they interpret nerve signals incorrectly, often leading to PN conditions. While this is still a new area of science, it is worth exploring if you are diagnosed with service-connected PTSD or TBI and are experiencing PN.
Alcoholism
Finally, alcoholism is a contributor to PN. Again, alcohol damages the peripheral nerves, reducing the blood flow and increases with extended use. However, many do not realize that often alcoholism is a secondary condition to a mental health problem that can be service connected. This is often worth filing a claim if there is a history of alcoholism that started in or after service.
Peripheral Neuropathy as a Secondary Condition
If a veteran is service connected for any of the conditions above, or wants to file for service connection for one of the conditions, and has peripheral neuropathy, it may be a secondary condition and may be worth filing a claim. Secondary conditions are often overlooked and can lead to higher ratings and increased benefits for veterans.