PTSD and Veterans: Breaking Down the Statistics
Because of the nature of their service, military veterans face particular risk of experiencing traumatic events and subsequently developing post-traumatic stress disorder (PTSD) symptoms. Drawing from the latest authoritative research, this page presents several important statistics pertaining to the incidence of PTSD among United States veterans.
You’ll also find helpful information related to the nature of the disorder, the mental health problems it causes, and how it can be effectively treated. Though post-traumatic stress disorder is alarmingly common among America’s veterans, there are valuable resources, treatments, and mental health care available to those recovering from military-related trauma.
PTSD Statistics: Prevalence Among Veterans
Though many researchers have sought to understand the prevalence of PTSD among military veterans, their efforts have produced divergent PTSD statistics. Because the field of psychiatry has defined and assessed PTSD in various ways over time, estimates of prevalence vary widely.
In fact, in one recent meta analysis of thirty-two scientific articles, researchers found the estimated incidence of PTSD among veterans ranged from modest figures such as 1.09% to high rates 34.84%. Clearly, determining the true prevalence of PTSD among veterans will require much further research.
However, some high-quality studies may shed some light on the matter:
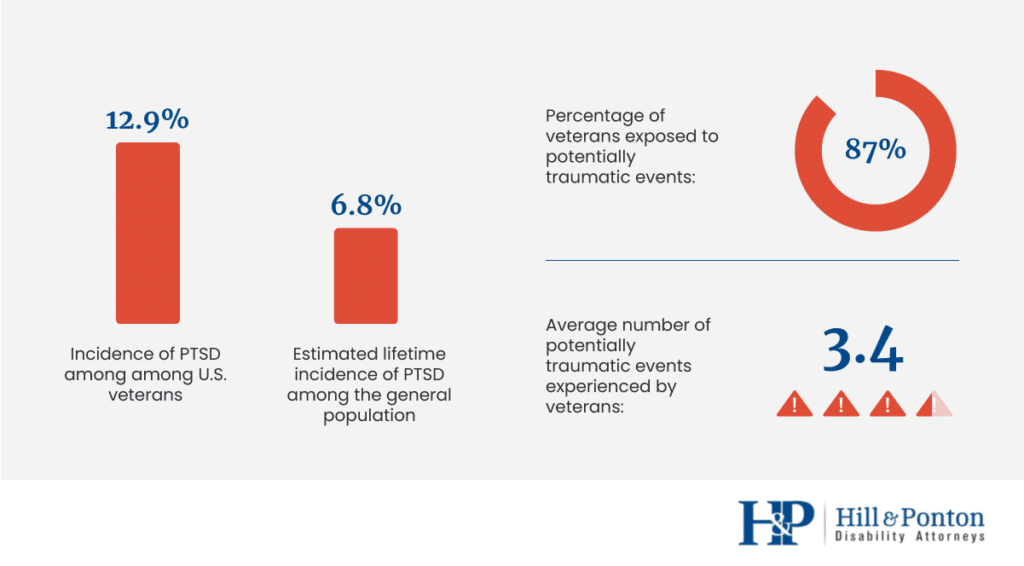
- In a 2017 study involving 5,826 United States veterans, 12.9% were diagnosed with PTSD. This is a striking high rate compared to the incidence of PTSD among the general population: Just 6.8% of the U.S. population will experience PTSD at any point in their lives. Across the entire U.S., only about 8 million U.S. adults have PTSD in a given year.
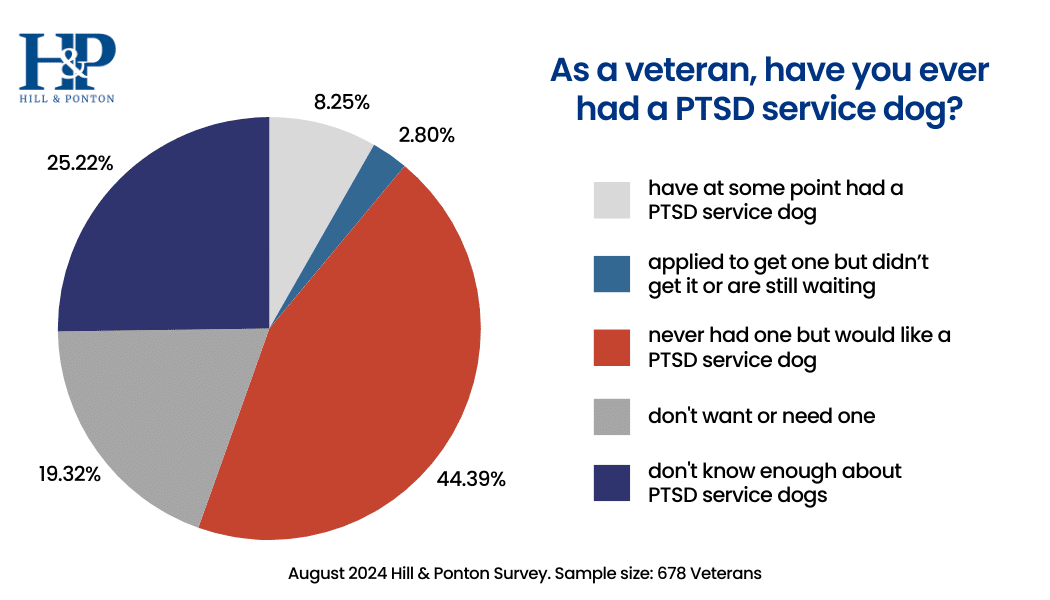
- In a 2014 study involving 3,157 United States veterans, 87% reported exposure to at least one potentially traumatic event. On average, veterans reported 3.4 potentially traumatic events during their lifetime.
PTSD Symptoms: What Affected Veterans’ Experiences?
Individuals with PTSD experience a diverse array of symptoms, and veterans with a diagnosis of PTSD may face several kinds of challenging thoughts and feelings. However, PTSD is generally characterized by a few distinct categories of symptoms, which mental health professionals use to assess and treat the disorder. These symptom categories, as described in the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM-5), capture the kinds of mental health problems that veterans with PTSD experience to differing degrees. These DSM-5 diagnostic criteria for PTSD are widely accepted in psychiatry and related mental health fields. To understand the daily struggles that PTSD can entail – or to assess whether you might be experiencing this condition yourself – consider the following:
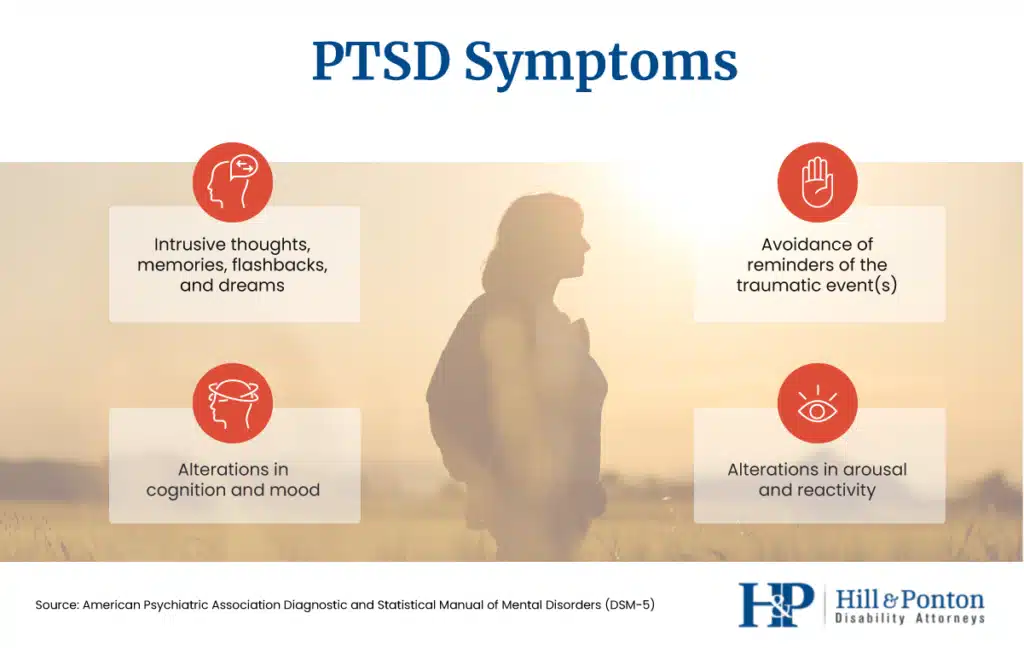
Intrusion of Thoughts, Memories, Flashbacks, and Dreams
This category, sometimes called “re-experiencing symptoms,” describes any kind of repeated, unwanted recollection of the traumatic events in question. These “intrusive” forms of thinking include memories and dreams, which can often be quite vivid. In some cases, individuals with a diagnosis of PTSD experience “flashbacks” in which they feel as if they are witnessing or reliving the traumatic event again.
For veterans, intrusive thoughts might include memories, dreams, or flashbacks of distressing combat experiences. Similarly, disturbing recollections of injuries or fatalities might repeatedly or unpredictably intrude on their thoughts.
Avoidance of Reminders of Traumatic Events
Because recalling traumatic events can be emotionally distressing, many individuals with PTSD avoid people, places, or things that might remind them of these experiences. Either intentionally or unconsciously, people with a diagnosis of PTSD typically steer clear of stressors that might “trigger” the painful thoughts and feelings associated with their trauma.
Among veterans with PTSD, this avoidance might involve resisting discussion of their military service or withdrawing from friendships with fellow service members. Post-deployment, veterans may rebuff questions from family members and loved ones about their combat experiences.
For many veterans with PTSD, seeking help may be extremely challenging, as doing so will likely involve direct discussion of their trauma. This barrier, coupled with our culture’s general stigma regarding mental illness, causes far too many veterans to avoid the mental health care they need.
Alterations in Cognition and Mood
Traumatic experiences can produce a complex mix of cognitive and emotional consequences. Veterans with PTSD can experience some or all of the following disruptions in their moods and thinking patterns, and these symptoms may combine to reinforce one another.
- Difficulty remembering certain details of the traumatic event
- Negative beliefs about oneself, others, or the world more generally, such as “I’m a bad person,” “I’m a weak person,” or “People can’t be trusted”
- Inaccurate, self-loathing, or self-blaming thoughts about the cause or nature of the traumatic event, such as “I could have prevented this,” “I caused this,” “I should have been able to save him,” or “I should have died instead”
- Feelings of guilt, shame, fear, or horror in connection with the negative thoughts and beliefs noted above
- Feelings of detachment or estrangement from others
- An inability to experience positive emotions such as contentment or happiness, even when circumstances would seem to warrant them
Alterations in Arousal and Reactivity
In individuals with PTSD, the brain and body experience a continued sense of danger long after the actual threat has passed. In particular, the amygdala, the region of the brain that processes fear and emotion, remains unusually active – as if life-threatening danger remained present.
Accordingly, veterans with PTSD may experience an ongoing sense of being “on guard,” which mental health experts term “hypervigilance.” This heightened awareness and reactivity to one’s surroundings can translate to the following difficulties, either while on active duty or post-deployment:
- Irritability or a propensity to angry outbursts
- Reckless, dangerous, or self-destructive behavior
- Being easily startled
- Excessive wariness regarding one’s environment
- Problems with attention or concentration
- Difficulty sleeping
PTSD Time Frame: How Symptoms Develop and Last
In the days immediately following a traumatic event, people often experience symptoms similar to those described above. However, PTSD involves the sustained presence of these mental health problems over a longer period.
In order to meet diagnostic criteria for PTSD, veterans’ symptoms must last for at least one month; often, they persist for years. Additionally, symptoms do not necessarily begin immediately following the trauma. While most individuals with PTSD experience symptoms within three months of the traumatic events in question, symptoms can also appear post-deployment. For veterans with PTSD, symptoms may emerge weeks or months after a period of combat or active-duty service.
PTSD Risk Factors for Veterans
Which factors increase a veteran’s risk of developing PTSD? Despite the significant advances in modern psychiatry, research into this question is ongoing. Much remains to be discovered about the biological and psychological determinants of PTSD in active-duty and former military personnel. Additionally, little is known about relative risks for various branches of the military, such as the U.S. Army, Navy, Air Force or Marine Corp.
However, a comprehensive meta analysis published in 2015 suggests that certain variables may influence a veteran’s likelihood of developing PTSD. These include the following:
- Degree of exposure to combat
- Discharging a weapon during combat
- Witnessing life-threatening injuries or death while deployed
- Levels of social support following traumatic exposure (such as the support of friends and family members).
Importantly, factors contributing to the onset of PTSD are highly ambiguous and individualized. There is no single definite way to determine the causes of this disorder in each case.
Rates of PTSD among Veterans by War
Some research suggests that rates of PTSD differ among veterans who served in different military conflicts. Indeed, there is compelling statistical evidence that military personnel who served in certain wars were somewhat more likely to develop PTSD symptoms.
- Vietnam War Veterans: The National Vietnam Veterans Readjustment Study, conducted from 1986 to 1988, found that 15.2% of men and 8.1% of women who served in Vietnam met diagnostic criteria for PTSD. Additionally, the estimated lifetime prevalence of PTSD was 30.9% among men who served in Vietnam and 26.9% among women. In a more recent study, researchers also found that PTSD was more prevalent among Vietnam veterans who had served in the theater of combat.
- Gulf War Veterans: In a study of over 11,000 Gulf War veterans conducted from 1995 to 1997, researcher Han K. Kang and his colleagues found that 12.1% had PTSD at the time they were surveyed.
- Iraq and Afghanistan Veterans: In a 2008 study, researchers at the RAND Corporation analyzed the psychological health of 1,938 veterans of Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF). OEF commenced in Afghanistan in 2001, whereas OIF launched in 2003. Among these veterans, 13.8% met criteria for PTSD at the time they were assessed.
Non-Combat Causes of PTSD Among Veterans
While many veterans experience PTSD following a traumatic event during combat, members of the military may also be exposed to other forms of trauma. According to the American Psychiatric Association’s diagnostic criteria, for example, one form of trauma that may prompt PTSD is learning of the violent death of a close friend. For military personnel deployed to combat zones, this kind of devastating experience could occur when a friend is killed in action.
Additionally, “repeated or extreme exposure to aversive details of the traumatic event(s)” could also produce PTSD symptoms. A military doctor, for example, might experience cumulative trauma after treating a series of combat wounds.
Unfortunately, there is yet another potentially traumatic threat to those who serve in the military: sexual assault.
Sexual Assault in the Military
Sexual misconduct is disturbingly common within the United States military. In fact, the U.S. Department of Veterans Affairs coined the term “military sexual trauma” to describe all forms of sexual assault or harassment experienced during military service. Survivors of these acts of sexual aggression often experience PTSD, as do survivors of sexual assault in civilian life.
Statistics pertaining to sexual assault in the military are alarming, including the following data points:
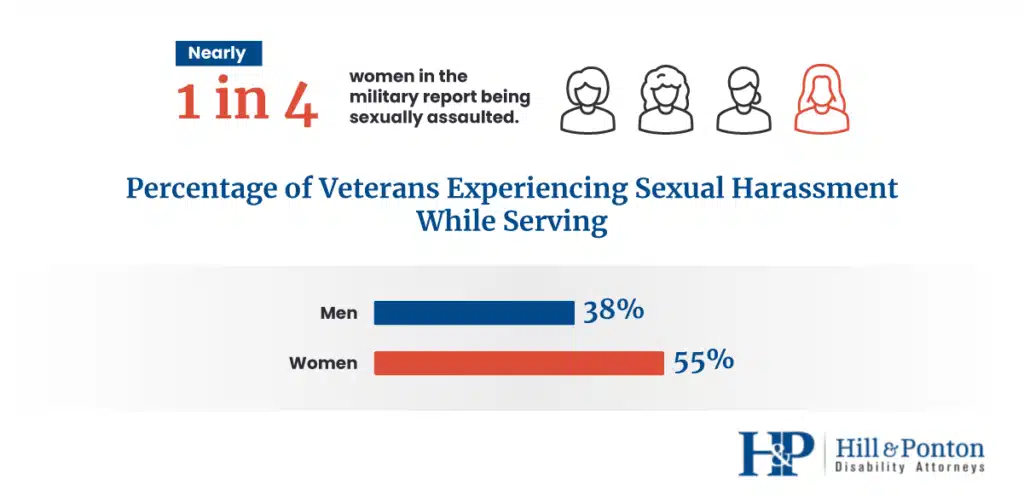
- Twenty-three percent of female veterans reported sexual assault while serving in the military.
- 55 percent of female veterans and 38% of male veterans experienced sexual harassment while serving in the military.
- Though stereotypes suggest survivors of sexual assault are predominantly female, more than half of veterans with military sexual trauma are men.
Trauma stemming from sexual harassment and assault can be no less devastating to veterans than experiences of combat, and prevention is a stated priority for U.S. Department of Defence. Additionally, VA health care facilities often offer services specifically designed for veterans who were sexually assaulted while serving.
Veterans with PTSD: Associated Health Risks
While the symptoms of PTSD can prove overwhelming in their own right, the condition is closely linked to other health risks in epidemiological research. Veterans who experience PTSD are at elevated risk for several related physical and psychological challenges. In some cases, the connection between these health problems is well understood; in others, the basis of the relationship requires further exploration.
Some of the health problems linked to PTSD, either in research pertaining specifically to veterans or among individuals with PTSD more generally, are as follows:
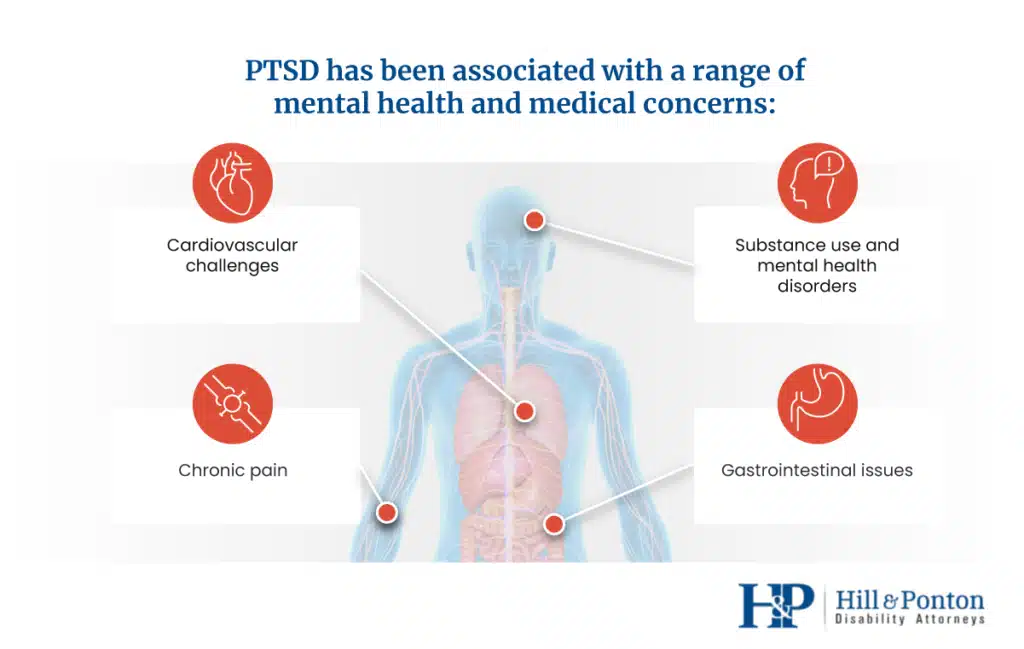
Mental and Behavioral Health Issues
- Substance Use Disorders: More than 20% of all veterans with PTSD also struggle with substance abuse challenges, referred to clinically as “substance use disorders.” Among veterans of the Iraq and Afghanistan war, for example, 63% diagnosed with substance abuse problems were also diagnosed with PTSD. The connection may relate to coping: Substance abuse may represent a means to manage distressing thoughts and feelings related to experienced trauma.
- Other Mental Health Disorders: Among people diagnosed with PTSD, roughly 80% meet diagnostic criteria for at least one other form of mental illness. Veterans are no exception to this troubling pattern. Many military service members with PTSD also experience depression and anxiety among other conditions. Additionally, some research indicates that veterans with PTSD are at increased risk of committing suicide, particularly if they experience combat-related guilt.
Medical Issues
- Cardiovascular problems: Several studies suggest a correlation between PTSD and poor cardiovascular health. This link has been consistently asserted in research involving both veterans and civilians with PTSD. Indeed, one analysis of 200,000 veterans found that those with untreated PTSD face a 24% to 46% greater risk of hypertension.
- Gastrointestinal issues: PTSD is associated with a range of gastrointestinal troubles, including serious conditions, such as irritable bowel syndrome. Initial research indicates that PTSD may actually alter the function of gut bacteria utilized in digestion.
- Chronic pain: Recurring physical discomfort and PTSD can become deeply intertwined, especially for veterans who sustain injuries during their active-duty service. In fact, among chronic pain patients, approximately 35% meet criteria for PTSD. Unfortunately, lingering pain can often serve to remind veterans of their traumatic experiences, exacerbating their PTSD symptoms.
- Traumatic Brain Injury (TBI): Due to the nature of modern warfare, military personnel now experience high rates of traumatic brain injuries. While a TBI may be relatively mild (such as a minor concussion), some research suggests that suffering any TBI during active duty elevates a soldier’s risk of developing PTSD. Additionally, because the psychological consequences of a serious TBI can include disruptions in mood and memory, differentiating PTSD from these symptoms can be a challenge for clinicians.
PTSD Treatment for Veterans: Effective Approaches
Thankfully, there are several effective and evidence-based forms of mental health care designed to treat veterans experiencing PTSD. In fact, the U.S. Department of Veterans Affairs has been a driving force in the development and testing of many PTSD treatment modalities, and VA health care facilities offer a wide spectrum of mental health services. Veterans interested in their mental health treatment options should consult resources available on VA.gov, including pages compiled by the VA’s National Center for PTSD.
Recent research suggests that psychotherapy is the most effective “first-line” approach to treating PTSD. Psychotropic medications may also be helpful, particularly when combined with talk therapy approaches. Additionally, some studies indicate that veterans with PTSD may benefit from coping methods that they can practice independently, without clinicians present.
Trauma-Focused Therapy Approaches
The following psychotherapy approaches are strongly recommended by either the American Psychological Association (APA.org) or the U.S. Department of Veterans Affairs (VA.gov) as PTSD treatment options.
- Cognitive Behavioral Therapy (CBT): This approach emphasizes how thoughts, feelings, and actions influence one another. The goal is to develop new patterns of thoughts, emotions, and behaviors pertaining to the traumatic experience and related subjects. Cognitive therapy, a related approach, focuses specifically on altering painful memories and evaluations related to the trauma that hinder daily functioning.
- Cognitive Processing Therapy (CPT): This modality aims to help individuals develop new, more helpful understandings of their traumatic experiences through critical reflection.
- Eye Movement Desensitization and Reprocessing (EMDR): This form of therapy involves recalling the trauma while paying attention to a back-and-forth movement or sound controlled by the clinician.
- Prolonged Exposure (PE): This approach emphasizes incrementally challenging negative feelings and altering patterns of avoidance stemming from one’s trauma.
Other therapeutic interventions may also prove effective in specific cases, so please seek the clinical expertise of a mental health professional if you are interested in learning more. Appropriate clinicians to contact regarding PTSD treatment include counselors, social workers, psychologists, psychiatrists, and nurse practitioners specializing in psychiatry.
Medications for PTSD
Some psychotropic medications have been demonstrated to be effective treatment options for people with PTSD. These prescription medicines can be combined with psychotherapy in a multifaceted approach to PTSD treatment.
The four medications with the strongest clinical support belong to the class of pharmaceuticals termed “antidepressants.” They include the following medications:
- Fluoxetine (Prozac)
- Paroxetine (Paxil)
- Sertraline (Zoloft)
- Venlafaxine (Effexor)
If you are interested in medication to treat PTSD, please contact a qualified medical professional for additional guidance. Please note, however, that medication is typically recommended in conjunction with other mental health services.
Coping Methods for Managing PTSD Symptoms
Beyond formal mental health care approaches, several “self-help” methods may prove valuable in managing PTSD symptoms. These practices are widely recommended by mental health experts as solutions that veterans can utilize in their spare time or when exposed to particular stressors. These techniques may be suggested as a complement to ongoing mental health treatment.
- Physical activity: Exercise can help relieve stress and elevate one’s mood.
- Aromatherapy: Certain smells, such as orange essential oil, may mitigate negative emotions associated with PTSD.
- Mindfulness practices: From formal meditation to simply noticing one’s senses, practicing being present can reduce trauma reactivity.
- Deep breathing:This seemingly simple technique can be surprisingly effective, and is available anytime, anywhere.
Veterans and PTSD: More Research and Resources
We hope you’ve found the PTSD statistics and research presented on this page to be helpful. To learn more about how PTSD affects veterans and for more access to crucial resources, visit the links below.
Age, PTSD, & Your VA Disability Claim