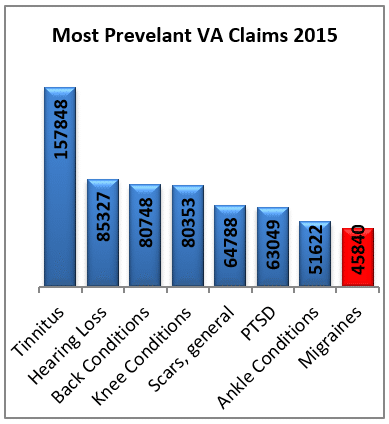
There are many different events that cause PTSD. Some examples are personal trauma, sexual trauma, combat, reactions to training. It is the 6th highest rated disability among veterans. There were over 63,000 new claims in 2015. VA compensates more than 800,000 veterans for symptoms of PTSD at some level. Many veterans have treating doctors who diagnose them with PTSD only to have VA turn down their claim. Even though these veterans submit all the evidence required. A lot of times, they see on their rating decision, “Does not meet the criteria for PTSD.” In this blog, we will explore reasons why veterans get denied and what they can do about it.
Incorrect Rating Decisions:
Often the rating decision is just incorrect. VA fails to grant PTSD cases but it also fails to consider other issues. VA denies a mental health disorder because the veteran filed for one disorder and actually has a different one.
Veterans, unless they have a doctorate in psychology, are not able to officially diagnose their own mental health disorders. Therefore, when a veteran claims PTSD VA can deny it But VA must see if he has another condition. VA should determine if the veteran has another diagnosis, which it often does not do. Veterans can often avoid this process by filing a claim for a more generic issue such as “acquired psychiatric disorder.” Another option would to be to file for “service-connected mental health disorder.” By filing for benefits in this manner, VA is responsible to diagnose and/or use medical records.
Understanding Criterion A of PTSD

This is one of the most puzzling aspects of diagnosing for lay people. Criteria A determines if a stressor supports a diagnosis of PTSD. If there is no Criteria A, there is no diagnosis. However, many people, even doctors, often misunderstand the requirements for this diagnostic step. The criteria broken down are:
What kinds of stressors support a VA diagnosis of PTSD?
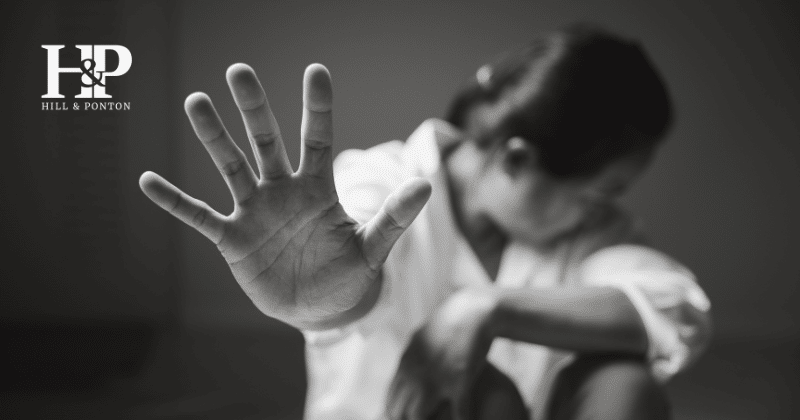
Exposure to actual or threatened death, serious injury, or sexual violence in one (or more) of the following ways:
- Directly experiencing the traumatic event(s);
- Witnessing, in person, the event(s) as others suffered occurred trauma;
- Learning that a close family member or close friend suffered a traumatic event(s). In cases of actual or threatened death of a family member or friend, the events(s) must have been violent or accidental.
- Experiencing repeated or extreme exposure to aversive details of the traumatic event(s) (e.g. first responders collecting human remains; police officers repeatedly exposed to details of child abuse.)
What if I didn’t see the death or trauma, can I still have PTSD?
For many, the basic criteria listed above of 1 and 2 are easy to understand. Where we find mistakes most often are with criteria 3 and 4.
Criteria 3 states that a family member or close friend must have suffered the event. Often, VA determines members of a unit are not close friends. VA justifies this by finding that they didn’t served together for a certain period of time. Another reason VA uses is that the servicemembers were not in the same place when the incident happened. VA ignores, however, the culture of the military, which follows no temporal or geographical bounds. Even if unit members are on different continents, they are bound by a brotherhood. When members of a unit experience a trauma such as terrorism or a plane crash, the entire unit is affected. This is true from those who directly experienced the trauma to support staff and support units.
VA often mistakes Criteria 4 as relating to repeated events only such as military security forces or convoy personnel. However, reading the criteria closer, it states, repeated or extreme. Extreme can mean a lot of things in the military world, terrorism, or IEPDs. It could even mean having to write up the reports dealing with the death or losses of troops or civilians. And, extreme is about perception. What may be extreme for one may not be perceived as someone else. So, discussing the events with a psychologist is important. A psychologist can determine how the veteran perceived the event and if it meets Criteria A requirements for PTSD.
Understanding the General Rating Formula for Mental Health Conditions
VA determines Rating levels by using the General Rating Formula. This is where VA takes the symptoms of any mental health condition and translates them into a rating. For PTSD, VA has ratings of 10, 30, 50, 70, or 100%. VA often rates veterans by the average of their symptoms. So, if a veteran has symptoms that fall in the 30, 50, and 70% ranges, they will often get a 50% rating. However, this is not the correct way to rate a mental health disorder.
The basis of a ratings is the highest level of symptoms, not an average. So, if a veteran has 6 symptoms at 30%, 3 at 50% and 2 at 70%, a 70% rating is proper. Also, the VA cannot downplay symptoms and give them a lower rating. For example, if a veteran has suicidal ideations, that is a 70% rating. However, VA doctors sometimes states that the veteran does not have intent or that the ideations are fleeting. VA will sometimes grant a lower rating by minimizing the symptom all together. It is, nevertheless, a 70% rating if a veteran has suicidal ideations—no matter the frequency or intent.
One rating not on the PTSD scale is unemployability (IU). PTSD often causes veterans to not be able to work. VA calls this IU. If your PTSD causes IU you should file for that as well. It is basically another way to get 100% benefits.
If you struggle with mental health conditions, get the correct rating and the highest benefits you are entitled to. You deserve it for the price you paid to defend your country.