“I have chronic asthma, and I use two inhalers to manage my asthma. How much will the VA rate me for my asthma?”
This is a common enough question. The VA’s rating schedule has been well-equipped to address all possible disorders of the nose and throat.
There are so many kinds of respiratory conditions, however, and the severity can vary so greatly, that the VA most often uses pulmonary function tests (PFTs) as a basis for its rating criteria.
Here’s what former military service members should know about pulmonary function tests and VA disability benefits for respiratory disorders.
VA Rating for Respiratory Cancers based on the PACT Act
The Honoring Our PACT Act of 2022, officially known as the Honoring Our Promise to Address Comprehensive Toxics Act of 2022, has revolutionized how the VA addresses service connections linked to toxic exposure during military service.
Through this Act, the VA has enhanced the presumption of service connection for several health conditions.
What does this mean for veterans? Essentially, if you were exposed to specific toxins during your military service—as validated by your service record—you’re not required to demonstrate a medical link between your present diagnosis and that exposure.
One significant area that the Honoring Our PACT Act of 2022 targets is respiratory cancers.
This broad category encompasses any cancer associated with the respiratory system, such as:
- Lung cancer
- Tracheal cancer
- Laryngeal cancer
- Bronchial cancer
Beyond respiratory cancers, over 20 other health conditions, many being various cancers, are now recognized as presumptively linked to toxic exposure from burn pits for veterans serving during the Gulf War and post-9/11 periods.
Other conditions gain their presumptive status due to exposure to agents like Agent Orange, radiation, and other toxins from specific incidents and locations.
Even if your service record doesn’t allow you to benefit from this presumption, you can still pursue a direct service connection through the VA disability claims process. However, in this scenario, you’ll need to establish a medical connection between your service and your diagnosis.
Understanding Lung and Respiratory Cancers
Globally, lung cancer ranks as the second most diagnosed cancer and is the primary cause of cancer-related deaths. The top risk factor for lung cancer remains smoking. Prevention primarily involves abstaining from smoking and evading passive smoke exposure.
Typically, lung cancer symptoms manifest in the advanced stages and might include:
- Persistent coughing
- Blood in cough
- Difficulty breathing
- Chest discomfort
- Vocal hoarseness
- Unaccounted weight loss
- Pain in the bones
- Frequent headaches
Other respiratory cancers present symptoms akin to lung cancer. For instance, tracheal cancer might lead to symptoms like a persistent dry cough, breathing issues, hoarseness, and swallowing difficulty.
Laryngeal cancer can result in hoarseness, voice alterations, a persistent sore throat, ear pain, or the feeling of a throat obstruction.
Bronchial cancer symptoms might comprise persistent coughing, bloody coughs, and chest pain.
Diagnostic procedures for lung cancer can include CT scans, X-rays, sputum cytology, or biopsies.
Treatment plans vary based on factors such as overall health, cancer type and stage, and patient preferences.
Typical treatments might include surgery, radiation therapy, chemotherapy, radiosurgery, specific drug treatments, or immunotherapy.
VA Ratings for Respiratory Cancers
The VA provides guidelines for disability ratings for respiratory cancers under the Diagnostic Code in 38 CFR § 4.97, titled Schedule of Ratings – Respiratory System.
For active or malignant respiratory cancers, VA automatically assigns a 100% disability rating during the illness and for six months post successful treatment.
After this timeframe, the VA arranges a C&P exam to evaluate your health and subsequently modify your rating. If your cancer enters remission, the VA will base the rating on any residual effects of your illness.
Types of Respiratory Disorders
Pulmonary function disorders are grouped into two main categories: obstructive and restrictive.
Routine spirometry testing measures two basic components: (1) air flow and (2) volume of air out of the lungs.
Putting it simply, if the air flow is impeded, the defect is obstructive. If the volume of air is reduced, the defect is restrictive.
Most respiratory disorders are grouped under one of these two categories. However, there several respiratory disorders do not fall under either of these categories, such as:
- Tuberculosis
- Pulmonary vascular disease
- Bacterial infections of the lungs
- Mycotic lung diseases (fungal)
Obstructive Disorders
Obstructive disorders make it difficult to exhale all the air in the lungs.
Damage to the lungs, or narrowing of the airways (bronchii) inside the lungs, cause air to be exhaled more slowly than normal.
This is due to reduced elasticity of the lung airways, or some kind of obstruction (like mucus or inflammation).
Obstructive lung diseases make it more difficult to breath, especially with increased activity of exertion.
As the rate of breathing increases, there is less time to breathe out all the air before the next inhalation.
Common obstructive disorders include:
- Chronic Obstructive Pulmonary Disease (COPD), including emphysema and chronic bronchitis
- Asthma
- Bronchiectasis
- Cystic Fibrosis
Restrictive Disorders
Restrictive disorders make it difficult to fill lungs with air.
This type of lung condition is a result of the lungs being restricted from fully expanding.
Usually restrictive diseases occur when there is stiffness in the lungs themselves.
Sometimes this can occur when there is stiffness in the chest wall, weak muscles or damaged nerves that restrict the expansion of the lungs.
In some cases (interstitial lung diseases), autoimmune or rheumatologic diseases can cause progressive scarring of the lung tissue that lies in between and supports air sacs. Scarring causes stiffness in the lungs.
Common restrictive disorders include:
- Interstitial lung disease (such as pneumonia)
- Sarcoidosis
- Obesity
- Neuromuscular diseases, such as amyotrophic lateral sclerosis (ALS)
- Asbestosis
- Pulmonary fibrosis
- Sleep Apnea
VA Disability Pulmonary Function Tests
A pulmonary function test (PFT) measures how much air can be inhaled and exhaled, and how much carbon monoxide can enter the bloodstream within a certain period of time.
PFTs are non-invasive. A veterans doctor typically performs a pulmonary function test when initially diagnosing the condition, and then periodically afterwards to gauge the severity of the condition.
PFTs can determine whether an obstructive or restrictive disease is present, and also determine the location of a defect. A pulmonary function test measures three aspects of lung function:
- Spirometry
- Lung volumes
- Diffusion capacity of the lung
These measurements show how effectively you’re able to breathe and how well your lungs are able to deliver oxygen throughout the body.
What Can I Expect from Pulmonary Function Tests?
Your doctor will provide specific instructions to prepare for your pulmonary function test.
This will likely include avoiding alcohol, smoking, caffeine, and heavy exercise within the hours leading up to the test.
You should also have a light meal and limit fluid intake. Be sure to wear loose clothes so you can breathe comfortably.
Once you arrive at your appointment, your healthcare provider will talk you through the steps of the test.
How Spirometry Tests Work
The most common form of pulmonary function tests is spirometry.
Spirometry is the easiest, fastest, and most readily available method of function testing in outpatient clinics.
The VA rating system depends mostly on spirometry results when evaluating a respiratory disorder.
A spirometer is a hand-held device into which the individual breathes.
Usually a clip is placed on the nose to prevent any air from entering the nasal passages.
The patient takes a deep breath, and then exhales as hard as he/she can for at least 6 seconds (10 seconds being ideal).
A small machine records the strength of the exhalation.
Because the validity of the test depends on the participation of the patient, the test is repeated two to three times in order to obtain accurate results.
A spirometer has two main functions:
- It measures the forced vital capacity (FVC), which is the amount of air that can be forcibly blown out after deep inhalation.
- It also measures the forced expiratory volume in 1 second (FEV1), which is the amount of air that is forcibly blown out in the first second of the exhale. When expressed as a percentage of the “normal” averages, the FEV1 determines the degree of obstruction (if any) of the air through the lungs – mild, moderate or severe.
How correct breathing affects the test
The participation of the patient is incredibly important for spirometer testing.
It is a natural reaction to be hesitant about taking as deep a breath as possible or exhaling as hard as possible when taking the test.
The assumption can be that the weaker the breath, the more accurate the test will be. However, this is not the case.
If the patient does not inhale deeply enough, the FVC and FEV1 will be underestimated, and the test results may mimic a restrictive disorder (such as pleural effusion or fibrosis).
If the patient does not exhale hard enough, the FEV1 may be underestimated, and the result may mimic airways obstruction (such as a false positive for COPD or asthma).
In order to ensure that spirometry test results are interpreted in an accurate diagnosis, it is imperative that the patient inhale has deeply as possible, and then exhale as hard as possible for at least six seconds.
What Should I Be Looking for in My PFT Results?
Once you have completed pulmonary function testing, your results should be available to review.
However, they will be difficult for you to understand without a medical professional to interpret them for you.
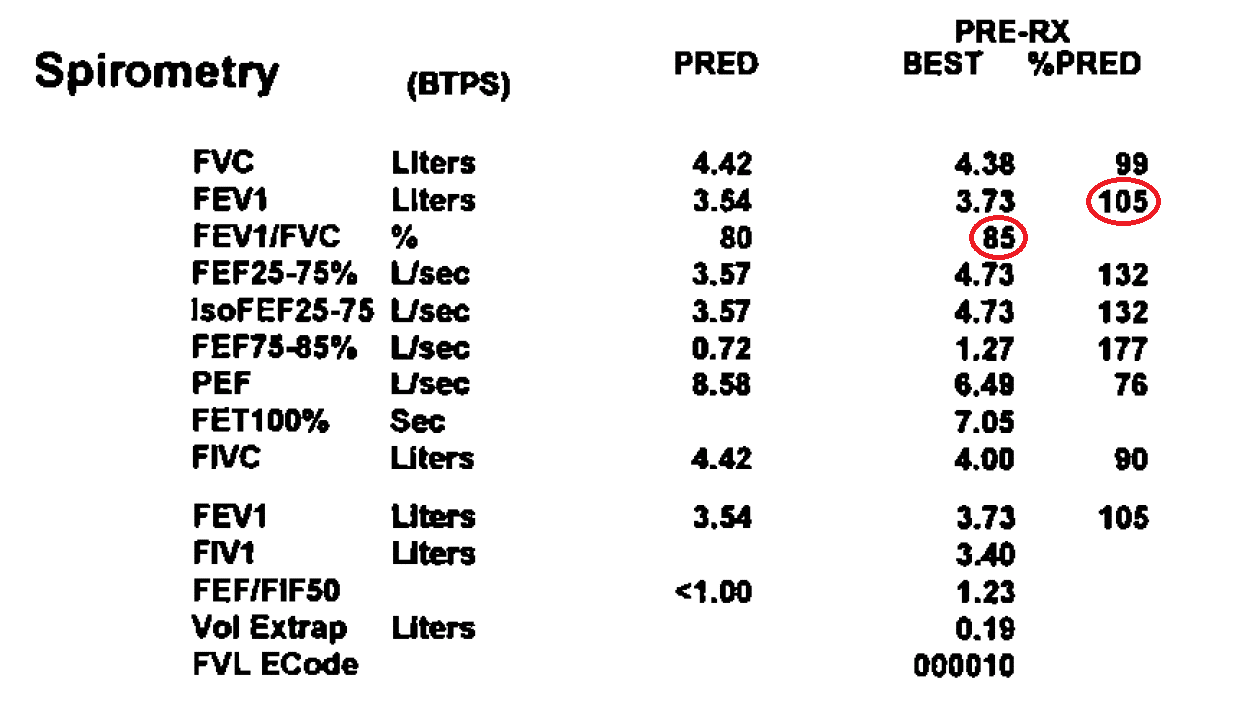
Spirometry results commonly look like the example below:
VA Disability Ratings for Respiratory Disorders
Once the VA determines service connection for the respiratory disorder, they will provide a rating based on the corresponding diagnostic code.
The VA rating schedule for respiratory disorders chiefly utilizes the numbers circled in the above example of a spirometry test.
The last three columns in the image above are the ones that we are concerned with.
Let’s break this down. And to make it easier, let’s call the patient “Bill.”
Useful Definitions
- PRED = the predicted value. This is the anticipated test result that a normal person (with no respiratory dysfunction) would have.
- BEST = the most accurate reading of the spirometry test. Usually the patient will take the spirometry test three times in order to obtain the most accurate representation of his/her condition.
- % PRED = a percentage representation of Bill’s test results relative to those of “normal” individuals with his ethnicity, height and build. For example, 85 % PRED would mean that Bill breathes 85% “normally.”
VA Ratings for Respiratory Conditions Explained
The VA uses 38 CFR § 4.97 – Schedule of Ratings – Respiratory System to rate pulmonary conditions.
This includes impairments of the lungs, bronchi, trachea, larynx, and more.
Let’s make sense of how the VA rates respiratory conditions like asthma.
Think of your lungs and everything connected to them—the pipes (bronchi and trachea), the voice box (larynx), and more.
A medical examiner will use a special chart to figure out how severe your condition is and what kind of compensation you should get.
Let’s take bronchial asthma as an example.
Quick Ratings Guide for Asthma
- 100% Rating: Your lungs are severely affected.
- You can only take in less than 40% of air in a deep breath compared to a healthy person.
- Your airflow (how fast you can breathe out) is less than 40% of what it should be.
- You’re facing severe asthma attacks more than once a week.
- You need strong daily meds (like high-dose corticosteroids) to manage.
- 60% Rating: Your asthma’s bad, but not the worst.
- You can take in 40-55% of air in a deep breath.
- Your airflow is 40-55% of normal.
- You need to see the doc regularly for flare-ups.
- You’re on strong meds three or more times a year.
- 30% Rating: Your asthma’s there, but it’s under control most days.
- You can take in 56-70% of air in a deep breath.
- Your airflow is 56-70% of normal.
- You’re using inhalers or meds daily to keep things steady.
- 10% Rating: Your asthma’s mild.
- You can take in 71-80% of air in a deep breath.
- Your airflow is 71-80% of normal.
- You only need inhalers or meds every now and then.
Now, let’s really simplify the 10% rating using an example.
Decoding the 10% Rating
Your doctor might give you numbers like FEV-1 or FEV-1/FVC after some breathing tests.
These are just fancy ways of measuring how much and how fast you can breathe out.
Let’s say, in your test:
- Line 2, Column 5 reads “105”. To get a 10% rating, this number should be between 71 and 80.
- Line 3, Column 4 reads “85”. To fit the 10% rating, this number should also be between 71 and 80.
From these two results, you wouldn’t qualify for a 10% rating.
But, if you occasionally use an inhaler, then you would still fit into the 10% category!
Remember, these ratings are all about understanding how your asthma or respiratory condition affects your life.
Talk to your doc, understand your numbers, and make sure you’re getting the support and benefits you deserve.
My breathing test results were normal, but I still have asthma. How is this possible?
Sometimes, spirometry test results create the appearance of a normal respiratory system.
In the example case described above, Bill’s high spirometry test results indicate that he can breathe perfectly well.
However, Bill suffers from asthma, needing an inhaler to manage periodic asthma attacks and shortness of breath.
So how is this possible?
Asthma is considered a reversible obstructive defect.
This means that the use of a bronchodilator (such as albuterol) can usually open up the airways and make it easier to breathe.
Most people with asthma can breathe fairly well unless they are having an active asthma attack.
Consequently, a spirometry test is more likely to be taken during a period of normal breathing, and will most not reflect a patient’s breathing pattern when having an asthma attack.
Therefore, when a diagnosis of asthma is suspected, the patient will be asked to participate in other tests that can more accurately pinpoint the problem.
What happens if my pulmonary function tests are outdated?
Some doctors may not require regular or extensive pulmonary function tests.
This can be a problem in terms of VA claims, since most of the rating schedules for respiratory disorders depend heavily on pulmonary function testing.
An outdated test will likely not be an accurate representation of the respiratory condition.
A similar problem exists in cases in which spirometry results indicate little or no respiratory dysfunction.
More advanced methods of pulmonary function testing, such as the measurement of lung volumes and diffusion capacity, may not be readily accessible in outpatient clinics and therefore not available the VA examiner’s review.
However, in the event that pulmonary function testing is not available or reflective the veteran’s actual condition, the VA offers another point of reference in the rating criteria—the use of medications for management of the condition.
Specifically, the rating criteria identify the use of corticosteroids (inhaled or oral), as in asthma cases, or the use of oxygen therapy, antibiotics, and immunosuppressives as reference points for the severity of the condition.
For example, if a veteran with asthma requires daily use of a bronchodilator inhaler to manage his asthma, he would be entitled to a 30% rating.
Whichever the case may be, the VA tries its best to cover every possible situation by the thoroughness of its Disability Benefits Questionnaire (DBQ) for respiratory disorders.
On examination of the patient, VA examiners are requested to indicate whether or not pulmonary function testing was performed, and if the testing accurately reflected the actual state of the veteran’s respiratory condition.
The DBQ also devotes a section for use of medications, bronchodilators, corticosteroids, antibiotics, and oxygen therapy that the veteran may be prescribed for the management of the respiratory disorder.
This questionnaire can also be completed by the veteran’s treating physician, as additional evidence in support of the veteran’s claim in the event that the C&P examiner was not sufficiently thorough or accurate.
Are you considering appealing for benefits for a respiratory disorder?
We may be able to help you with your claim. Fill out a case evaluation form for more information.